A team led by Vanderbilt University biomedical engineer Michael Miga, Ph.D., has been awarded a five-year, $3.1 million grant from the National Cancer Institute to enhance image-guided surgery techniques for safely removing liver tumors.
While aggressive surgery is a highly effective treatment, it risks injury to the liver, which can lead to post-operative liver failure.
The goal of the grant is to apply recent advances in image-guided surgery to the liver so that more surgeons can conduct safer, more aggressive resections that avoid blood vessels and other critical structures.
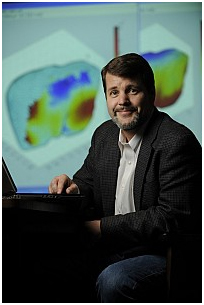 Biomedical engineer Michael Miga |
“We have one common tenet that drives everything,” said Miga, associate professor of Biomedical Engineering, Radiology and Radiological Sciences, and Neurological Surgery. “We are in the business of creating and translating technology to improve the care of the patients that walk through our doors today, not 20 years from now.’’
Miga’s co-principal investigators are William Jarnagin, M.D., vice chair of Surgical Services and chief of the Hepatopancreatobiliary Service at Memorial Sloan-Kettering Cancer Center in New York City, and James Stefansic, Ph.D., MBA, chief operating officer of Pathfinder Therapeutics Inc. in Nashville and a former research assistant professor at Vanderbilt.
Miga and Stefansic were among several Vanderbilt faculty members who co-founded Pathfinder Therapeutics in 2004.
Others included Bob Galloway, Ph.D., professor of Biomedical Engineering, Neurological Surgery and Surgery; Benoit Dawant, Ph.D., professor of Electrical Engineering, Biomedical Engineering, and Radiology and Radiological Sciences; Alan Herline, M.D., associate professor of Surgery and Biomedical Engineering; and Will Chapman, M.D., now at Washington University School of Medicine in St. Louis.
Starting with a versatile image-guided surgery system created by Galloway and his graduate students, the company has developed a “GPS” device for the surgeon. It involves the use of an optical probe during the operation to produce a map of anatomical “coordinates” on the surface of an organ.
A computer program “registers” or matches that information to a CT image of the organ taken before surgery.
This produces a “rigid registration,” which allows for the patient’s CT image to be projected onto a screen and actively visualized in the operating room to guide the surgeon.
The problem is that the liver is not rigid — its shape changes or becomes “deformed” during surgery. Miga has developed technology to compensate for the deformation. The new, non-rigid registration is more sophisticated, making it easier for the surgeon to steer clear of healthy tissue and focus on removing the tumor.
If the current research project is successful, it could lead to the first commercially available “soft tissue deformation correction system” for image-guided liver surgery, the researchers said.
“So many of our discoveries in science and engineering are challenged to make it out of the laboratory and help the patient,” Miga said. “The hallmark of this unique partnership grant will be its rapid translation framework. It is very exciting to be part of this effort.”
By Bill Snyder, VUMC News Service