
Graduate students Drew Harmata, left, and Jon Page with Professor Scott Guelcher, right. (Anne Rayner / Vanderbilt)
A pair of Vanderbilt graduate students has received a national award of $15,000 to pursue the development of an unique synthetic foam as a new treatment for deep skin wounds such as chronic foot ulcers caused by diabetes.
Drew Harmata and Jon Page, graduate students working in the laboratory of Scott Guelcher, associate professor of chemical and biomolecular engineering, were one of nine student teams that received awards in the second stage of a national competition, the National Collegiate Inventors and Innovators Alliance’s E-Team Program. Last year, the two won a first stage award of $5,000. By winning a stage two award this year, the team received $15,000 and qualified to compete in the third stage of the competition next year where they are given the opportunity to pitch their innovations to investors and can receive an investment up to $50,000.
The idea of commercializing the graft, which they have tentatively named PoraDerm, came when Harmata became involved with the Life Science Tennessee Academic Alliance, the student arm of a statewide non-profit organization established to advance the life science industry in Tennessee.
“I began looking at the various projects in our lab to see if any would make a viable product and start-up foundation, and identified PoraDerm, even though my Ph.D. thesis was not focused on skin regeneration,” said Harmata.
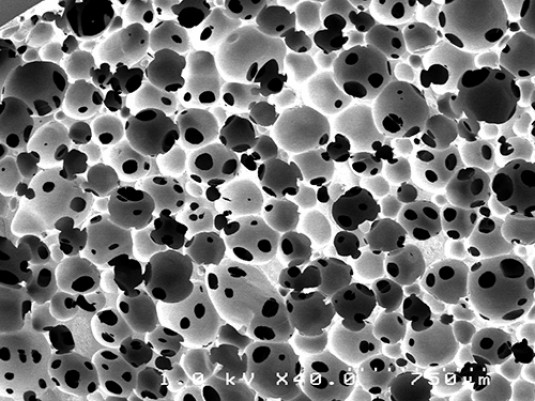
Microphotograph shows the porous structure of PoraDerm, a special type of biodegradable polyurethane. (Courtesy of Guelcher Lab)
According to Guelcher, the lysine-based polyurethane material was originally developed by a Japanese company as a clear coat for automobiles, but it proved to be too expensive for that application. However, the material had an unusual property which set it apart from the forms of polyurethane used in floor coatings and electrical insulation. It is non-toxic and biodegradable. This made it extremely attractive to researchers like Guelcher working in the area of tissue engineering.
“We’ve been working with this material for seven or eight years. We’ve tested it for a large number of applications and have applied for several patents,” said Guelcher.
One of their discoveries made in collaboration with professors Jeff Davidson and Lillian Nanney in the Vanderbilt University Medical Center was that the material is particularly effective at treating deep cutaneous wounds, and potentially chronic foot ulcers, which are responsible for more hospitalizations than any other diabetes complication. More than two million Americans suffer from chronic ulcers, requiring treatments that cost about $8 billion per year.
To treat such a deep wound, the rigid foam is shaped so it fits snugly into the defect. Once it is inserted, the material serves as a scaffold that holds and directs the new tissue as it grows into the opening. As the healthy cells spread, the foam degrades until it disappears completely when the wound is completely filled in.
The device must pass through an extensive FDA approval process before they can schedule clinical trials to compare its effectiveness to that of existing products.
“We know that this is just one small step in a long process, but we hope that PoraDerm will ultimately be used widely in the nation’s hospitals to help patients recover from their wounds,” said Harmata.