Trainees gain big picture knowledge plus work closely with surgeons

The results are in: Five cohorts of Vanderbilt engineering doctoral students have experienced ‘paradigm-shifting training’ in surgery and intervention.
Preliminary reports from a five-year program of intensive training, supported by a nearly $1 million National Institute of Biomedical Imaging and Bioengineering grant, show strong evidence that immersive levels of clinical contact resulted in significant improvements in the students’ understanding of procedural medicine and their ability to identify important questions that if solved would result in breakthroughs in clinical care. The agency has renewed the grant with another $1 million, five-year award.
Offered as a unique educational opportunity in the School of Engineering’s surgery and engineering research neighborhood and supported by the Vanderbilt Institute for Surgery and Engineering, the program is for second- and third-year engineering PhD students in biomedical engineering, electrical engineering, mechanical engineering, and computer science.

It includes sessions with surgeons and interventionalists who are researching and treating a myriad of conditions that involve over a dozen medical specialties that span procedural medicine. From brain tumor surgery and neuromodulation implants to robotic surgeries in the lung, prostate, and kidney, to arterial and ablation therapies in the liver and to radio-oncological procedures in breast and eye and more, the program adapts to contemporary treatment paradigms and strives to develop new understandings of disease and dysfunction by the studying of procedure.
“The engineering, surgery, and intervention ecosystem we have built at Vanderbilt is something wholly unique and with no parallels,” said Michael I Miga, Harvie Branscomb Professor, professor of biomedical engineering and VISE co-founder and Seminar Series Chair. “For near four decades, Vanderbilt has had this multi-generational professional fluidity among the medical center’s physicians and the university’s engineering faculty.
“Many institutions have engineers who collaborate with physicians; Vanderbilt is different, it’s much, much more,” Miga said. “There is this environment of exchange and support where if you can dream it, the expertise, infrastructure, and enthusiasm fall into place and the needle is pushed forward in clinical care with advances that are simply unmatched anywhere. Our training program is a core example of that environment.”
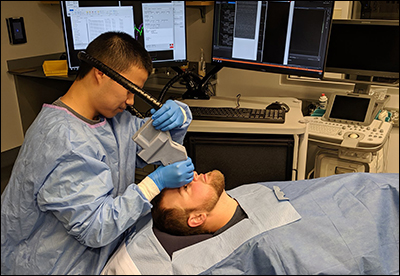
In the first of two courses in the program core, trainees attended lectures by 10 or more physicians who presented their procedural specialties interleaved with lectures on related engineering principles. A second course offered clinically-mentored immersion experiences in the operating room or interventional suite, at clinical conferences, and in patient rounds.
Real domain experiences
Miga calls this training approach “real domain experiences.” “Too often, rather than beginning with observations of clinical barriers, trainees are either introduced to a research laboratory’s perspective or are integrated into a standardized design framework. Exposure to ‘real-domain experiences’ has the goal of establishing an interactive dialogue in the context of clinical immersion where capability meets need with a better more unfettered exchange. Without these raw observational experiences, innovation may become inhibited and frankly we might lose out on some really exciting engineering ideas,” Miga said.

“Putting clinically naïve engineering students into interventional suites allows them to assess what is occurring with a fresh set of eyes. Their assessment often leads to ideas for further study that are not so apparent to the experienced clinician,” said co-PI Robert F. Labadie, professor of otolaryngology, head, and neck surgery and a Vanderbilt Institute for Surgery and Engineering affiliate.
“I was able to shadow a rheumatologist and multiple orthopedic surgeons in the clinic and operating room. I observed six joint replacement surgeries for knees, hips and shoulders, and I had the opportunity to interact with patients who suffer from osteoarthritis and other joint diseases,” said trainee Carli DeJulius,

“This experience was invaluable to shaping my perspective of my project to keep patient needs and clinical translation in mind. Without this program, my knowledge of the disease and treatment would be purely theoretical. I feel very fortunate to have had this opportunity,” said DeJulius, whose research focuses on drug development for osteoarthritis. DeJulius is a fourth-year biomedical engineering Ph.D. student in Professor Craig Duvall’s Advanced Therapeutics Laboratory.
Immersive clinical contact works
In this first 5-year cycle, trainee improvements were assessed in their ability to pose important questions in surgery and intervention, their knowledge of surgical technologies, and their understanding of procedural medicine.
Results are reported on quantitative experiential clinical involvement and on a self-reported survey of 18 trainees:
- With respect to immersion, the number of surgeries/interventions observed, the number of different types of procedures, and the clinical contact time per student was on average 15+ surgeries/interventions, 8+ different types, and 48+ clinical contact hours.
- With respect to trainee understanding of procedural medicine, surgical technologies, and value of clinical observation, an average perceived improvement of 41%, 38%, and 41% over the training course core was reported.
- Equally impressive, when rating ability to pose important questions affecting human health, an average perceived improvement of 34% was reported.
“There is a lot of big-picture knowledge you gain: workflow, patient experience, existing technology in the operating room. But the true value extends well beyond that. The opportunity to work closely with clinicians throughout my training has provided me with invaluable knowledge in developing technology that will easily integrate into the operating room,” said Winona Richey, a fifth-year BME graduate student.

“There are smaller, and more abstract things you pick up on that really frame how you think about a problem: What is the layout of our operating rooms and what is the footprint of personnel and current technologies? Are there parts of the clinical workflow that could be modified for better patient care?” Richey said.
“It was my experience in clinical interactions that really sparked my interest in incorporating subsurface features into our modeling approach,” Richey said. “Almost all patients have biopsy clips implanted near the tumor, but most have a separate localization device implanted as well. Shouldn’t we be able to just leverage those biopsy clips for localization? If we could, that would eliminate a second, painful procedure for the patient, and for the clinic, it would save a lot of time and scheduling headaches.”
Richey said to design novel solutions that will be adopted, it’s important for engineers to truly understand the big picture of these procedures from the perspective of both clinicians and patients. “After shadowing in the clinic and the operating room for several months, I was able to develop a prototype image guidance system for breast conserving surgery that our collaborators were very excited about.”
Miga said clinical immersion for traditional graduate engineering education is not common but is essential in order to advance procedural medicine. “With the organic development of this surgery and engineering neighborhood over decades at Vanderbilt, the training grant represents a codification of that ecosystem and provides a blueprint for enabling others to adopt similar frameworks,” he said. “With such integration, the technological advances to patient care in the next century will be better than any science fiction fantasy you find in your favorite books.”
Miga and Labadie reported on the program this summer in the new Springer journal Biomedical Engineering Education, the official educational journal of the Biomedical Engineering Society.
The grant number is T32EB021937.
Contact: Brenda Ellis, 615 343-6314
brenda.ellis@vanderbilt.edu