We spend nearly one-third of our lives asleep, yet sleep disorders often go undiagnosed, despite their strong links to cardiovascular disease, neurological disorders, and depression. A next-generation wearable device developed by researchers could change that.
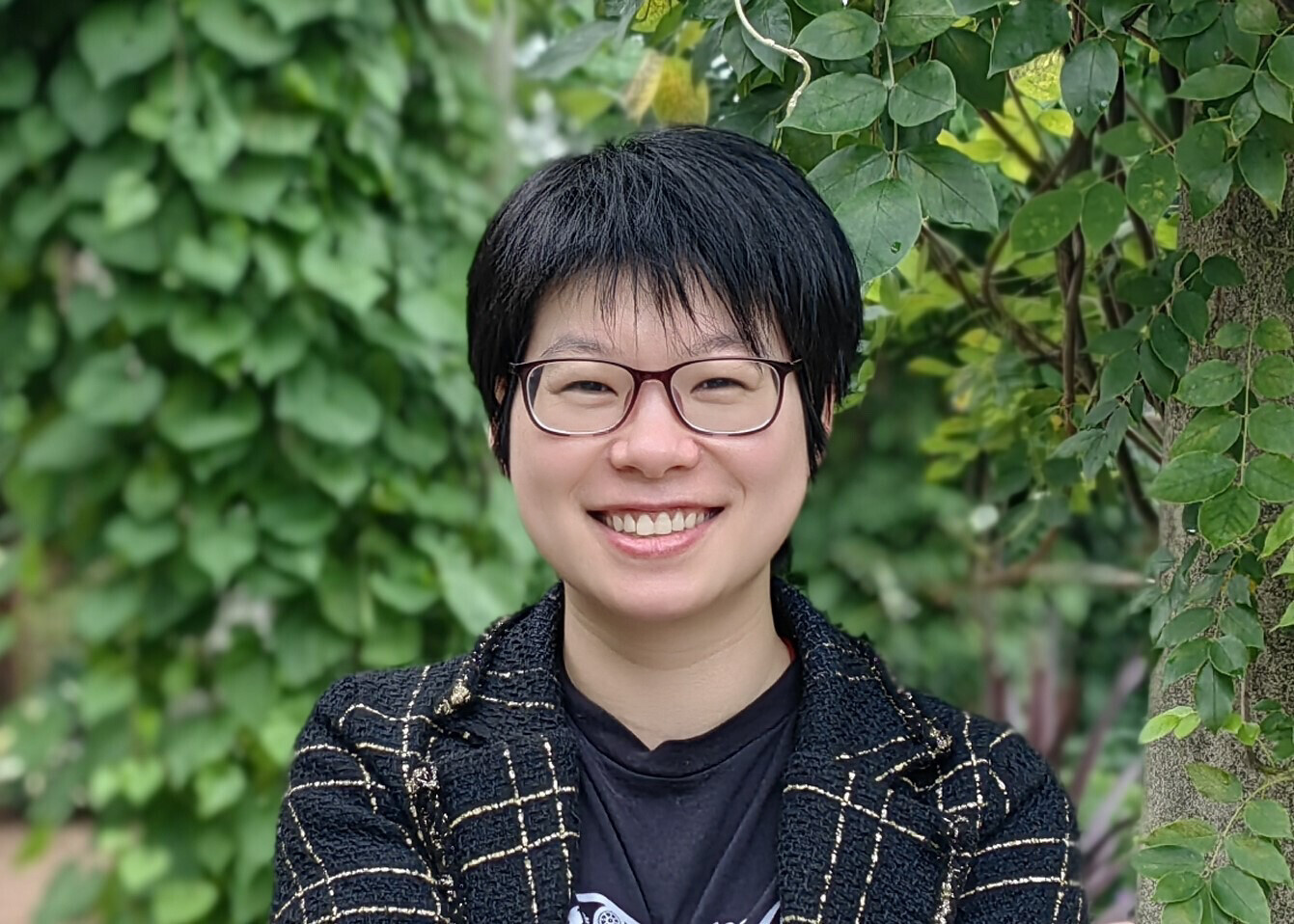
Yayun Du, assistant professor of electrical and computer engineering at Vanderbilt University, is the lead author of a pioneering study, “A skin-interfaced wireless wearable device and data analytics approach for sleep-stage and disorder detection,” published in the Proceedings of the National Academy of Sciences (PNAS) on June 6, 2025. The study describes a novel skin-interfaced, wireless sleep monitoring system that combines multimodal sensing with explainable artificial intelligence (AI) to improve the detection of sleep stages and disorders, including sleep apnea.
“Accurately identifying sleep stages is critical for diagnosing and managing a wide range of chronic conditions,” said Du, who is also part of the Vanderbilt Institute for Surgery and Engineering. “But most consumer devices don’t measure the most informative signals—particularly breathing, limiting their precision in detection of sleep stages and sleep disorders.”
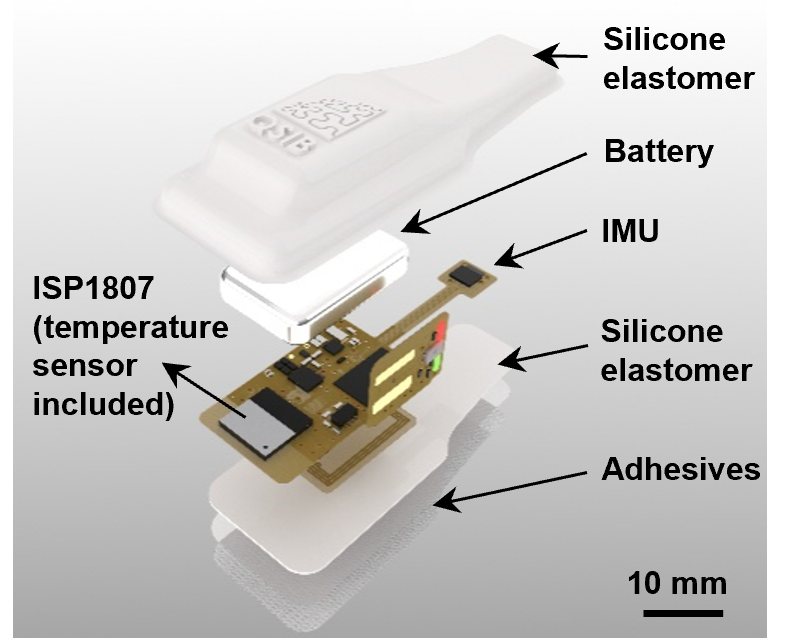
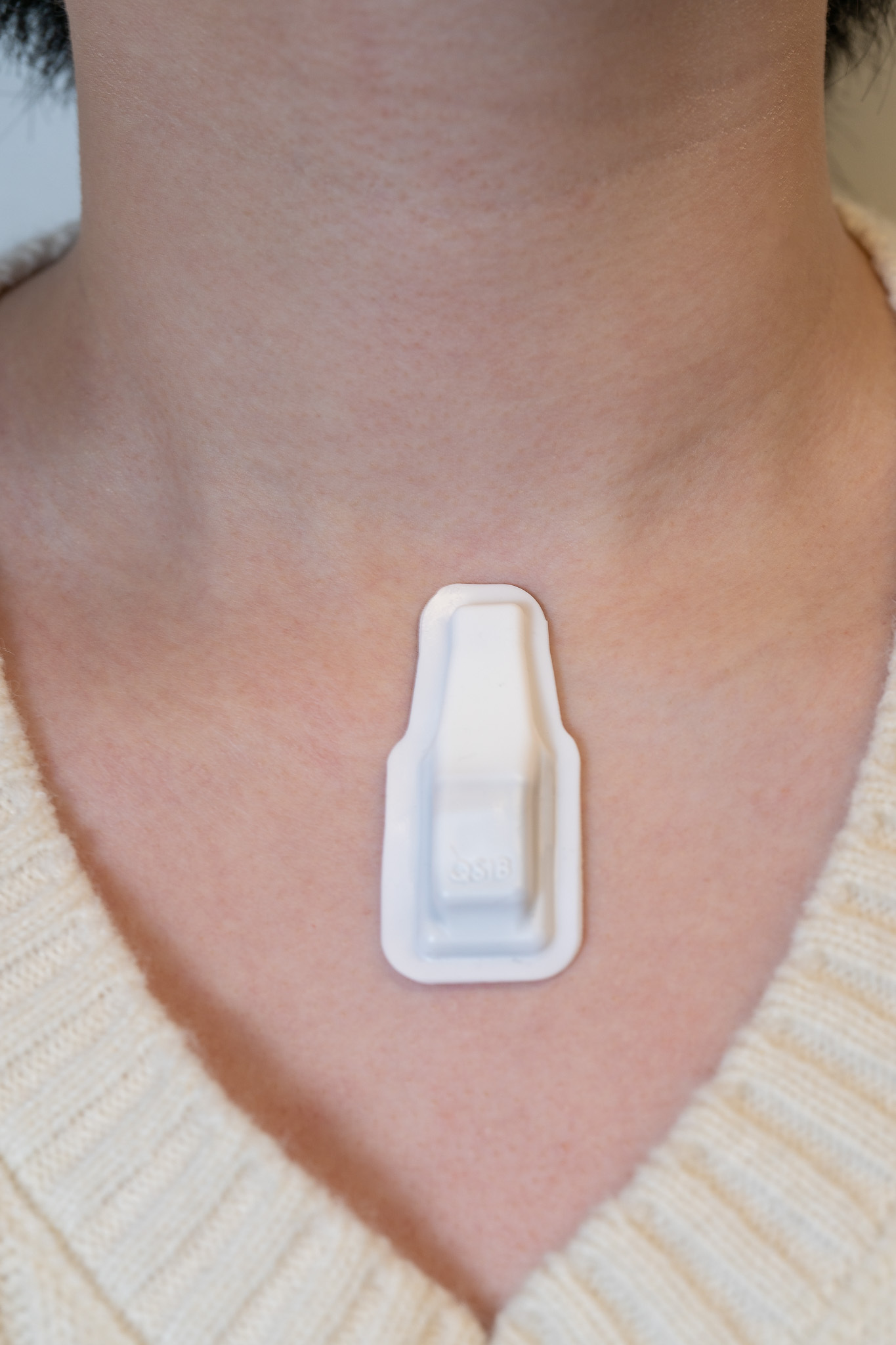
Unlike traditional wrist- or finger-worn trackers that rely on indirect signals, the new device features a soft, skin-mounted, energy-efficient sensor capable of directly measuring both respiratory and cardiac activity. This mechanoacoustic sensor captures detailed multimodal physiological data, including breathing rate, heart rate and variability, temperature, and body motion, all while being comfortable enough to wear overnight and several days per wireless charge.
The device wirelessly transmits data via Bluetooth to a machine learning framework called LMA-SleepNet, which analyzes over 140 features extracted from the signals. The system delivers personalized, interpretable sleep scores and disorder predictions directly to a user’s phone or tablet, giving both patients and physicians unprecedented visibility into sleep health.
In 2022, the American Heart Association introduced an updated metric called Life’s Essential 8, with sleep as a key factor in assessing cardiovascular health. Insufficient and low-quality sleep leads to decreased labor productivity and higher mortality rates, according to the association.
“What sets our device apart isn’t just where it’s worn—it’s how smart it is,” Du explained. “Breathing patterns, more than any other signal, turned out to be the most reliable markers of REM sleep and wake transitions—something conventional devices often miss.”
The research was conducted in collaboration with John A. Rogers and his team at Northwestern University, and supported by the Querrey Simpson Institute for Bioelectronics at Northwestern and the Procter & Gamble Company.
Contact: Lucas Johnson, lucas.l.johnson@vanderbilt.edu