As a child, Jenna Dombroski was at her grandfather’s bedside when cancer took his life. A scientist, he was her inspiration. Years later, the Vanderbilt University Ph.D. student and National Science Foundation Graduate Research Fellow is honoring him by leading the development of what appears to be a promising treatment for breast cancer metastasis, and potentially other types of cancer.
“He encouraged us to pursue exciting and interesting careers, and I always liked science and engineering,” says Dombroski, whose field of study is biomedical engineering. “His death to cancer had a lasting impact, and I’m grateful for the opportunity to combine science and engineering in research to fight the disease, and hopefully save lives.”
The research led by Dombroski in the lab of Michael King, J. Lawrence Wilson Professor of Engineering and chair of the biomedical engineering department, has found that vaccinations of tumor nano-lysate (TNL) – cancer cells broken up into thousands of nanoparticles – delay primary tumor growth and metastasis after being challenged with a tumor cell implantation.
The study builds on years of King’s research on circulating tumor cells (CTC) – how cancer cells travel throughout the body in the bloodstream – and the initiation of apoptosis by the protein TNF-related apoptosis-inducing ligand (TRAIL). TRAIL, combined with fluid flow, acts as an explosive, rupturing individual cancer cells into thousands of nanoparticles.
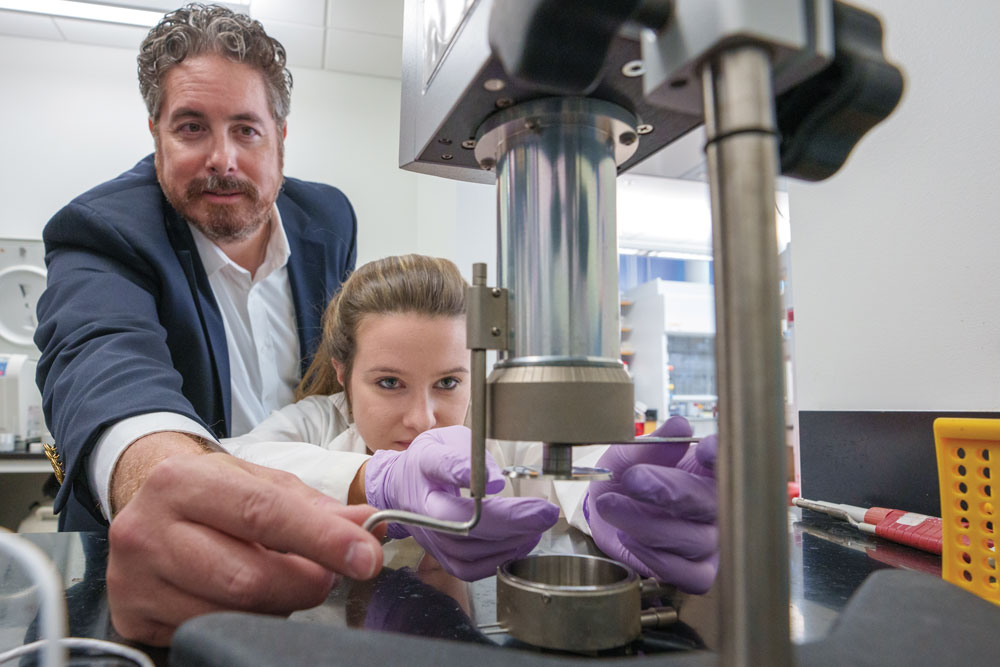
In the lab, Dombroski and King recreated the apoptosis effect without using TRAIL at all. Instead, the duo found the precise conditions required of ultrasound forces to recreate how the protein breaks apart the cancer cells into TNL. Working in the Vanderbilt Institute of Nanoscale Science and Engineering Analytical laboratory, Dombroski and King mimicked the effect down to the exact size, shape, protein composition, and electrostatic charge. The TNL was then injected into mice, and much like any other vaccine that trains the immune system to recognize and attack foreign viruses or bacteria, the native white blood cells not only responded to the TNL but learned to smash the CTC responsible for metastasis.
Dombroski says it is exciting to see the intersection of science and engineering in the TNL research.
“The engineering behind our project is that we’re modifying cancer cells by disrupting the cell membrane via applied ultrasonic waves,” she says.
Cancer vaccine research is a rich and active field, and international research teams are working on a number of complicated processing techniques. A widely used approach consists of removing white blood cells to treat them outside the body and then reinserting them to see how they respond to cancer cells. The King Lab has made some exciting strides in this field through their novel research into activating T cells by exposing them to fluid flow as an improved way to train them to attack cancer cells once they are reintroduced to the body.
Dombroski says their research is also somewhat unique in that “there is really little characterization of these cancer cell lysates.”
“Our lab uniquely coined these as tumor nano-lysates for our vaccine, and we’re able to do that because they’re nanometer sized,” she says.
Their new technique gives the King lab the ability to optimize the vaccine by adding other chemicals to improve the efficacy of cancer immunotherapy and increase the trial size, which could lead to breakthroughs in addressing other types of cancer.
“What we want to do next iProfessor Michael King and Jenna Dombroski go over notes to plan next steps for TNL studies.s figure out why this approach works so well,” says King. “The why is important because it allows us to take a step back as engineers and see what we can do to make it better, to expand it. Right now, it’s just for triple-negative breast cancer, but it’s something that we can potentially extend to other cancers.”
According to the Centers for Disease Control and Prevention, in 2019, the most recent incidence data, 1.7 million new cases of cancer were reported in the United States, and nearly 600,000 people died of cancer. In the case of breast cancer, specifically, each year in the U.S. about 264,000 cases are diagnosed in women and about 2,400 in men. Roughly 42,000 women and 500 men in the U.S. die each year from breast cancer.
Survival rates for the localized disease are 99% but fall to 27% in the latest, metastatic stage. This is caused when a cancer cell from a static tumor leaches into the bloodstream as a CTC. While most CTC die, some are able to survive in the bloodstream long enough to land in a different part of the body and grow into a new tumor in a different organ.
“Breast cancer can be caught very early with just a regular checkup, but unfortunately the stats are still high,” says Dombroski. “However, the innovative research that we’re working on here at Vanderbilt offers hope, and reassurance.”
William Gradishar is director of the Maggie Daley Center for Women’s Cancer Care in Chicago, Illinois, and chair of the National Comprehensive Cancer Network (NCCN) guidelines panel for breast cancer. He says efforts to develop vaccines for breast cancer have been underway for decades with various platforms, and that the research at Vanderbilt is indeed promising.
“The research from Vanderbilt is encouraging based on laboratory models of a new technique (nanotechnology) to deliver a vaccine,” says Gradishar. “Only clinical trials in patients will determine if this strategy fulfills its promise.”
Unlike chemotherapy, which acts directly on cancerous tumors, immunotherapy treats patients by acting on their immune system. In order to destroy cancerous tumors, chemotherapy is intended to attack rapidly dividing cells within the body, which may include both cancerous and non-cancerous cells, such as hair follicles and the lining of the gut. These attacks on healthy cells may cause some of chemotherapy’s more well-known side effects, such as hair loss, nausea, and darkening of pigmentation.

John Wilson is associate professor of chemical and biomolecular engineering at Vanderbilt and an expert on cancer immunotherapy and the use of cancer vaccines. He was recently awarded grants to develop technology that seeks to boost a person’s immune system to better fight cancer.
Wilson says there is still much to learn about how mechanical forces influence the fate and function of immune cells, and how that knowledge can be leveraged to develop safer and more effective immunotherapies for cancer, but that Vanderbilt is poised and equipped to make breakthroughs.
“Vanderbilt has a super strong mechanobiology community that is ideally positioned to tackle these challenges and lead in this exciting new area of cancer research,” he says.