Vanderbilt researchers are bolstering the fight against cancer with technology that enhances the effectiveness of T cells that attack tumors. The cutting-edge research was recently published in the high-impact journal Science Immunology.
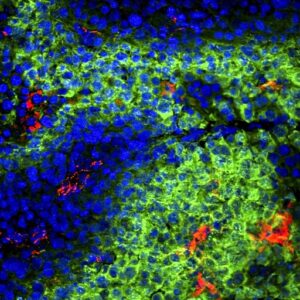
Cancers co-opt both the immune and cardiovascular systems to fuel their own growth, researchers say. They do this in part by forming new blood vessels that provide essential nutrients to rapidly dividing cancer cells. T cells in the immune system also use blood vessels as conduits for finding and invading tumors. But vessels in tumors are often abnormal and put up barricades that impede the ability of T cells to locate and kill cancer cells.
However, using a nanotechnology invented in the Immunoengineering Lab at Vanderbilt, researchers discovered they could reverse – or normalize – the malformed tumor vasculature by activating the stimulator of interferon genes (STING) pathway, a component of the immune system that plays an important role in protecting against pathogen infection and the development of cancers.
John T. Wilson, associate professor of chemical and biomolecular engineering at Vanderbilt and a corresponding author on the paper, said that the ability of the technology to reprogram the vasculature of tumors can help make T cells more effective at eradicating cancer cells.
“This allowed T cells to better infiltrate and destroy tumors in mouse models of kidney and breast cancer and enhanced the efficacy of immunotherapies that are currently being used in patients,” said Wilson, who is also Principal Investigator of the Immunoengineering Lab and a Chancellor Faculty Fellow.
In the publication, researchers also discuss testing their STING-activating nanoparticle (STAN) technology on tumors that had been surgically removed from patients with renal cell carcinoma (RCC). Consistent with findings from their experiments with mice, they found that STANs “demonstrated superior immunostimulatory activity,” offering “initial evidence supporting the potential use of STANs as a strategy to coordinate antitumor innate immunity and vascular remodeling in human RCC.”
Such breakthroughs are needed. This year, nearly two million new cancer cases and more than 600,000 cancer deaths are projected to occur in the United States, according to the American Cancer Society.
“While this technology isn’t yet ready for use in cancer patients, our study revealed an exciting new strategy for improving responses to cancer immunotherapy,” said Wilson.
Other co-authors on the publication include Lihong Wang-Bishop, Blaise Kimmel, Verra Ngwa, Matthew Madden, Jessalyn Baljon, David Florian, Ann Hanna, Lucinda Pastora, Taylor Sheehy, Alexander Kwiatkowski, Mohamed Wehbe, Xiaona Wen, Kyle Becker, Kyle Garland, Jacob Schulman, Daniel Shae, Deanna Edwards, Melissa Wolf, Rossane Delapp, Plamen Christov, Kathryn Beckermann, Justin Balko, W. Kimryn Rathmell, Jeffrey Rathmell, and Jin Chen.
Contact: Lucas Johnson, 615-343-0137
lucas.l.johnson@vanderbilt.edu