A multidisciplinary group of investigators from Vanderbilt University Medical Center, Vanderbilt University, and the University of Pennsylvania received a $3.2 million grant to develop novel brain network-based measures to guide surgical decisions and improve outcomes in the field of epilepsy surgery.
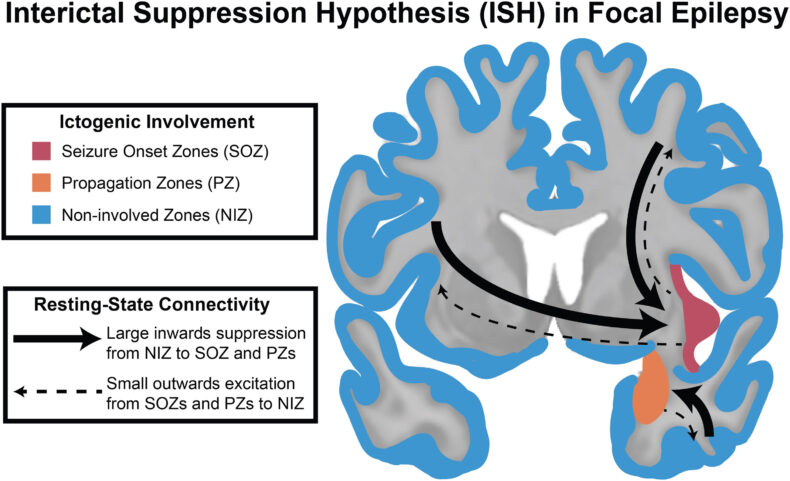
Epilepsy is a debilitating neurological disorder where seizures are often resistant to medications, but surgery can stop or reduce seizures and improve quality of life. However, the current clinical tools guiding surgical decisions are limited, in part because of an incomplete understanding of brain connectivity patterns in focal epilepsy.
The newly funded project will combine magnetic resonance imaging (MRI) structural and functional connectivity analyses with intracranial recordings and neurostimulation measures, including both hypothesis-driven and machine-learning based analyses. The goal is to develop new brain network-based tools that aid physicians around the country in improving patient selection and surgical outcome prediction as well as localization of surgical targets.
The five-year grant from the National Institutes of Health enables investigators from neurosurgery, neurology, radiology, biomedical engineering, electrical and computer engineering, and computer science to link expertise to improve patient lives. The project builds upon work recently published by VUMC investigators in the journal Brain.
The VU team is led by site principal investigator Benoit Dawant, PhD, MS, Cornelius Vanderbilt Professor of Electrical and Computer Engineering and director of the Vanderbilt Institute for Surgery and Engineering (VISE). Dawant brings expertise on atlas approaches and electrode localization. Catie Chang, PhD, assistant professor of Computer Science, will guide simultaneous EEG-fMRI and analyze arousal level analyses, and Mikail Rubinov, PhD, assistant professor of Biomedical Engineering, Computer Science, and Psychology, will lead advanced network analyses.
“Our traditional tools to determine where seizures start and to guide which surgery is best for an individual patient are imperfect and usually do not consider the brain network alterations that lead to epilepsy. Our goal is to develop novel network-based measures that can be applied broadly at epilepsy centers to guide surgical decisions and improve outcomes,” said Dario Englot, MD, PhD, principal investigator of the grant. Englot is an associate professor of Neurological Surgery and the director of Functional Neurosurgery at VUMC and leads the Brain Imaging and Electrophysiology Network (BIEN) laboratory.
Alongside Englot at VUMC are co-investigators Vicky Morgan, PhD, professor of Radiology, who will lead the fMRI expertise and connectivity analyses, Shawniqua Williams-Roberson, MD, assistant professor of Neurology, who will help define epileptic networks and outcomes, and Baxter Rogers, PhD, MS, associate professor of Radiology, for statistical modeling.
“This project is an excellent example of what VISE promotes and enables, with multi-institutional investigators in several engineering, basic science, and clinical departments all working together to solve an important clinical problem,” said Dawant.
At Penn, Kate Davis, MD, division chief of Epilepsy, is site PI to guide model validation with an external patient cohort.
The research is supported by the National Institute of Neurological Disorders and Stroke of the NIH under award number 1R01NS134625-01.
This story was adapted from The VUMC Reporter: https://news.vumc.org/2024/01/11/novel-brain-network-approach-to-improve-epilepsy-surgery/