Vanderbilt engineers have made a significant leap toward developing killer T cells to attack cancer tumors by “nudging” them into action with far less evidence of disease than previously thought.
Now, researchers will look for T cells that demonstrate potential for the strongest binding when they’re flung at damaged cells.
The work by Vanderbilt University Professor of Chemical and Biomolecular Engineering Matt Lang, Ph.D. student Yinnian Feng and their Harvard University collaborators appears in the Aug. 17 early edition of the Proceedings of the National Academy of Sciences.
Titled “Mechanosensing drives acuity of αβ T cell recognition,” the student is the result of more than 1,000 individual experiments aimed at triggering T cells when they are given a humanly undetectable push.
The research promises to change what immunologists are looking for, because it demonstrates that T cells can trigger killing of cells with far less evidence of infectious pathogens, physical damage and malignant transformations than researchers believed, Lang said.

“We can, for the first time, pick the closer on the baseball team who can reliably pitch fastballs,” Lang said. “Which T cell do you pick, which one do you put back into the patient to fight their disease? Maybe you get lucky and pick the right one. With these new tests, we can measure the interaction under the native, energized state. We’ve found the sweet spot for reliably triggering them.”
Scientists studying the body’s cancer-fighting T cells have had a serious hurdle: When they culture them in the lab, the T cells sit around at equilibrium, waiting to bump into cancerous cells. But once inside the body they act like motorized little bloodhounds, actively seeking out infected cells.
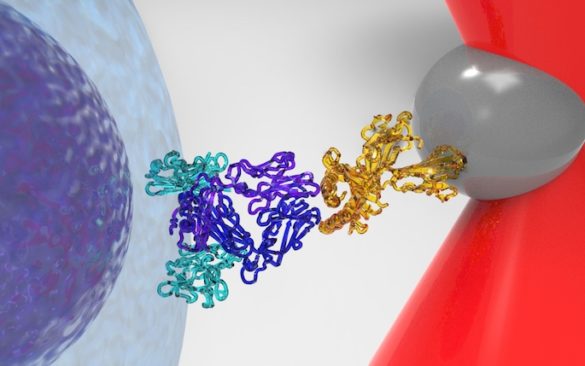
Feng and Lang performed their experiments using optical tweezers – highly focused laser beams – to pick up microscopic spheres and coat them with the same peptides as found on diseased cells. They would then place the spheres onto T cells.
With no force, the T cells were thought to go through their typical lab routine of lackadaisically sniffing out a peptide, then another, then another in a process requiring hundreds or even thousands of binding events before their receptors bound to enough peptides to activate the immune response.
Then Feng and Lang applied 10 piconewtons of force to the T cell, equivalent to the gravitational force exerted by dropping 1/1,000th of an eyelash. A special dye applied to the T cell immediately revealed an increase of intracellular calcium, which shows that it is activated. Feng and Lang began removing a peptide at a time as their experiments progressed and learned that, with this tiny amount of force, the T cell can do its job when contacting as few as two peptides.
“With the very precise microscopes we have, we didn’t see repetitive binding. We saw a single binding event,” Lang said. “This paper is telling us about mechanism, about how the system actually works. It’s basically saying that we’re dealing with a mechanosensor that requires force to be activated. Strategically, it’s changing what we should be looking for.”
He said the research has personal significance to him because his wife has fought thyroid cancer for years—she is currently cancer-free—and he’s lost other relatives to cancer in quick succession.
Lang’s team collaborated with Harvard’s Dana-Farber Cancer Institute, where researchers have been studying T cell receptors that distinguish abnormal cells from normal cells since the early 1980s. Dr. Ellis Reinherz said he worked with Lang when the engineering professor was at MIT, just prior to Vanderbilt.
“What Matt has shown here is that, in the presence of force, the ability of a T cell to recognize its target is dramatically enhanced,” Reinherz said. He warned against treating the new research finding as a panacea, but characterized it as enormously important fundamental science.
“This sort of technology will be useful in honing our way of best identifying tumor antigens and developing rational methods of discerning T cell receptors one from another on bond strength,” Reinherz said. “We may be able to improve the quality we’re generating, characterize them and define with great authenticity pathogen-derived responses. Our work is fundamental to developing antigen-specific, killer T-cells.”
The team’s work could help with designing strategies for T cell therapies, said Dr. Christian S. Hinrichs, an investigator with the National Cancer Institute.
“In the emerging and very promising field of T cell therapy, these findings help us understand at a very basic level how therapeutic T cells are triggered to attack their targets,” he said.
The research was supported by NIH Grants R01AI100643 and SU2C-AACR-DT1314.
Media Inquiries:
Heidi Hall, (615) 322-NEWS
heidi.hall@vanderbilt.edu